An In-depth Interview with Kris Newby, Author of “Bitten”
“We need to let the NIH know that we’re watching them, and we want results.”
– Kris Newby
 Kris Newby, author of ‘Bitten,’ is investigating government spending on Lyme disease research, which is strongly influenced by the flawed original disease definition of Lyme disease. She summarizes the impact of the 2018 Tick-Borne Disease Working Group’s report, explains where research funding has and is currently being directed, and calls for money to be spent on better diagnostics and treatments for Lyme disease sufferers instead. Kris explores potential actions that Lyme patients can take to help direct the course of funding, such as communicating with Congress, supporting advocacy groups, and donating to research organizations.
Kris Newby, author of ‘Bitten,’ is investigating government spending on Lyme disease research, which is strongly influenced by the flawed original disease definition of Lyme disease. She summarizes the impact of the 2018 Tick-Borne Disease Working Group’s report, explains where research funding has and is currently being directed, and calls for money to be spent on better diagnostics and treatments for Lyme disease sufferers instead. Kris explores potential actions that Lyme patients can take to help direct the course of funding, such as communicating with Congress, supporting advocacy groups, and donating to research organizations.
The views and opinions expressed in this article are those of the interviewee and do not necessarily reflect the views or positions of Bay Area Lyme Foundation.
Kris Newby is watching our government, and watching quite closely. She has a lot to say about how government money is spent on a disease that, according to CDC estimates, infects almost 500,000 people annually in the US, causing untold pain, suffering, loss of livelihood, and, in extreme cases, severe mental illness, including suicidal and homicidal events.
Of course, we are talking about Lyme disease—the pariah of infection-associated chronic conditions.

 “I want to leave you with hope. I think we’re going to be unstoppable because I think that these are solvable problems. These are answerable questions. I think that there are already a lot of existing tools in immunology that just need to be brought into the fight, and we can change this.”
“I want to leave you with hope. I think we’re going to be unstoppable because I think that these are solvable problems. These are answerable questions. I think that there are already a lot of existing tools in immunology that just need to be brought into the fight, and we can change this.” 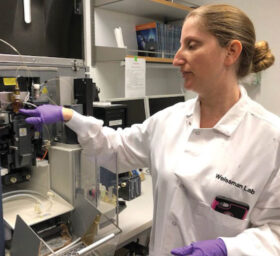 Any respectable pathogen that can establish a persistent infection needs to figure out your immune system to the point that it can evade it. The fact that it has persisted means that it was able to evade your immune clearance. And so, I got to that from a very interesting direction working on immune regulation, trying to understand these brakes on the immune response and how they impact the response to infection. The immune system has the power to kill you and obviously, nobody has any incentive for that to happen. So, there are a lot of mechanisms in place to put brakes on the immune system and reign it in. One of the huge developments in cancer over the last two decades has been reevaluating the question: can we take those brakes off? So in my postdoc, I was studying a particular checkpoint where this was turning into an exciting immuno-oncology target, and I said, ‘I want to look at how this checkpoint is used in infection.’ I realized that this checkpoint was being used to help you survive an acute infection, but created a vulnerability for pathogens to evade immune clearance and establish chronic infection much like it allows cancer cells to evade immune clearance. In an amazing collaboration with Irv Weissman, Balyn Zaro, and Jenifer Coburn we realized that the bacteria that cause Lyme disease manipulate this brake and that’s how I became fascinated with Lyme. But I also became concerned about turning off this brake in cancer patients because I was concerned about what would happen if you used this on cancer patients during an active infection. Indeed, the
Any respectable pathogen that can establish a persistent infection needs to figure out your immune system to the point that it can evade it. The fact that it has persisted means that it was able to evade your immune clearance. And so, I got to that from a very interesting direction working on immune regulation, trying to understand these brakes on the immune response and how they impact the response to infection. The immune system has the power to kill you and obviously, nobody has any incentive for that to happen. So, there are a lot of mechanisms in place to put brakes on the immune system and reign it in. One of the huge developments in cancer over the last two decades has been reevaluating the question: can we take those brakes off? So in my postdoc, I was studying a particular checkpoint where this was turning into an exciting immuno-oncology target, and I said, ‘I want to look at how this checkpoint is used in infection.’ I realized that this checkpoint was being used to help you survive an acute infection, but created a vulnerability for pathogens to evade immune clearance and establish chronic infection much like it allows cancer cells to evade immune clearance. In an amazing collaboration with Irv Weissman, Balyn Zaro, and Jenifer Coburn we realized that the bacteria that cause Lyme disease manipulate this brake and that’s how I became fascinated with Lyme. But I also became concerned about turning off this brake in cancer patients because I was concerned about what would happen if you used this on cancer patients during an active infection. Indeed, the 
 Lyme Disease Biobank established a key partnership with the nonprofit
Lyme Disease Biobank established a key partnership with the nonprofit  “Although it is an emotional and difficult idea for anyone to plan to donate parts of their body to science after they have died, we believe that this decision is an important way for Lyme patients to change the course of Lyme disease research. Having access to tissues from the brain, heart, joints, and central nervous system of Lyme patients allows researchers to prove unequivocally that Lyme is present in tissue and contributes to patient suffering,” explains
“Although it is an emotional and difficult idea for anyone to plan to donate parts of their body to science after they have died, we believe that this decision is an important way for Lyme patients to change the course of Lyme disease research. Having access to tissues from the brain, heart, joints, and central nervous system of Lyme patients allows researchers to prove unequivocally that Lyme is present in tissue and contributes to patient suffering,” explains 
 Charlotte Mao:
Charlotte Mao:

 Sunjya Schweig, MD, founder of the
Sunjya Schweig, MD, founder of the 

