 Erythema migrans (EM, literally means “expanding rash”) is the hallmark sign of infection with B. burgdorferi. Most rashes occur 3–30 days after infection, however there are case reports that show EMs can appear sooner than three days post infection.
Erythema migrans (EM, literally means “expanding rash”) is the hallmark sign of infection with B. burgdorferi. Most rashes occur 3–30 days after infection, however there are case reports that show EMs can appear sooner than three days post infection.
The Centers for Disease Control and Prevention report that as many as 80% may exhibit the erythema migrans, but this number can vary by region and study.
For example, a 2010 study showed that in the state of Maine only 43% of Lyme patients exhibited the erythema migrans. In 2019, the California Department of Public Health Annual Report cited only 33% exhibited the EM. Furthermore, in a study by Dr John Aucott in the Mid Atlantic area, only 20% of EMs had the bullseye presentation.
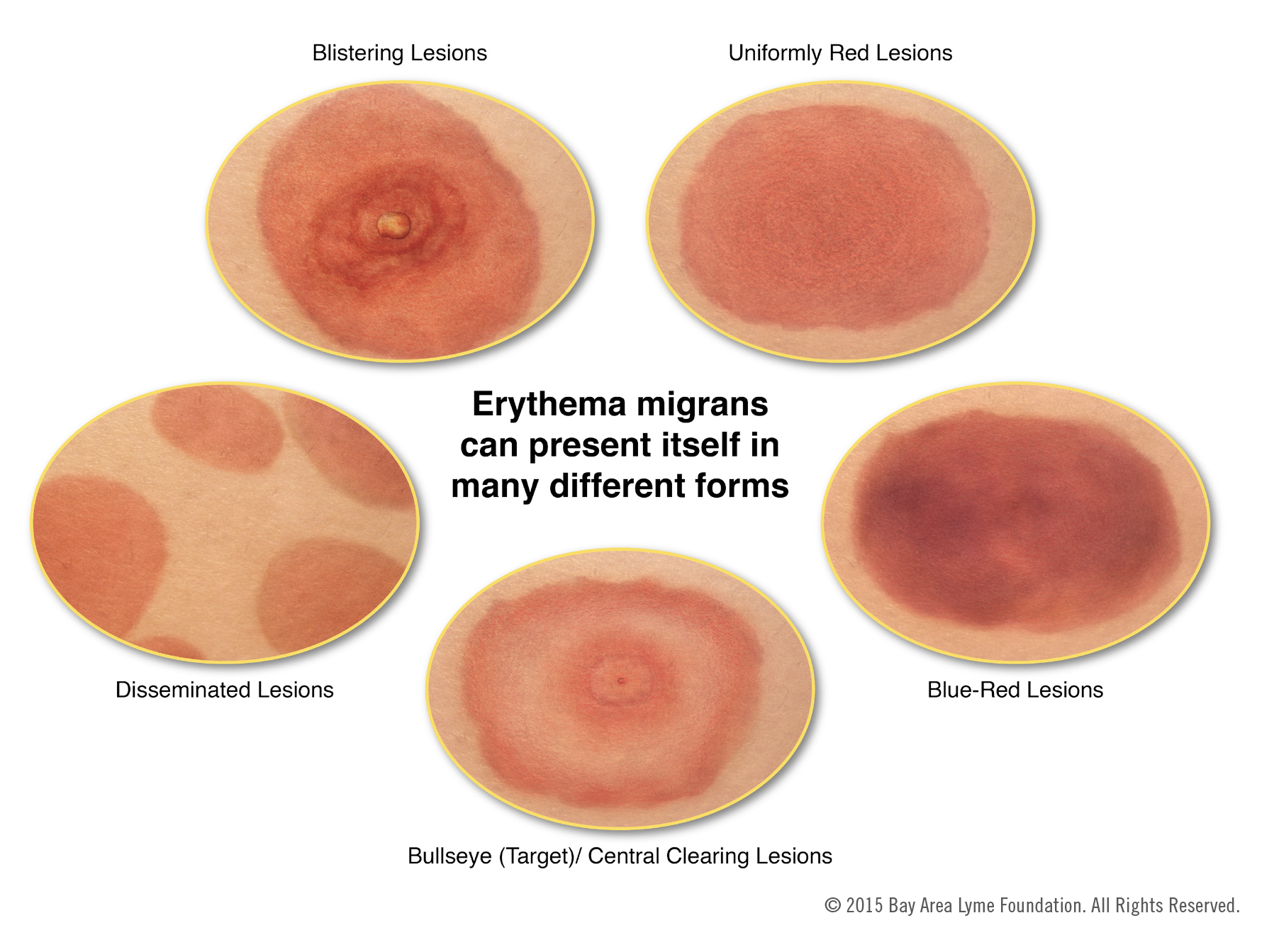
While many equate a Lyme rash with the bulls-eye, this is not the definition of an EM. An EM is defined as an expanding annular (round) rash of at least 10cm (2.5in). The rash can take many forms, and may have a raised bump in the middle, can be itchy or warm, and can have a bluish cast like a bruise. The rash may not be present at all. You should also watch for other symptoms.
If you have a rash, the best thing is to document it—take a picture next to a ruler so you can determine the size. This can be very helpful to a healthcare provider in evaluating the rash. You can also draw a ring around the contours to see if it expands over time.
If you see multiple EM rashes (these can form close to the original rash, or in other places) this indicates a disseminated infection. Again, take a picture of the rashes and get in touch with your healthcare provider immediately. Disseminated infection means the infection has circulated in your body and could be present in the brain, the heart and/or the joints. Immediate treatment with antibiotics is important to prevent more severe complications of infection, like Lyme neuroborreliosis or Lyme carditis.
The chart below illustrates several of the forms these rashes might take.
There are many symptoms of Lyme disease and it is critical that you are alert to all of them. See Lyme Disease Symptoms for more information.
Don’t Be Fooled
Lyme disease is often referred to as the great imitator because so many of its symptoms resemble those of other diseases. Without a telltale skin rash, it can be very hard to diagnose Lyme disease. Many people never recall being bitten.
Below is a list of just some of diseases that many people have initially been diagnosed with, only to receive a Lyme diagnosis later:
- Cellulitis: bacterial infection involving the inner layers of the skin which presents with a erythematous rash similar to a Lyme disease erythema migrans rash
- Arthritis: typically manifesting as joint pain, swelling, redness, heat, and limitation of movement
- Juvenile idiopathic arthritis: a childhood disease that causes joint inflammation and swelling
- Fibromyalgia: especially widespread muscle and soft tissue pain
- Chronic fatigue syndrome: severe and debilitating fatigue
- Multiple sclerosis: leading to problems with muscle control and strength, vision, balance, sensation, and mental functioning
- Lupus: joint pain, swelling, may affect kidneys, brain and other organs
If you suspect Lyme, even if you do not recall being bitten, try to recall where and when you might have been exposed to infected ticks, and discuss the situation and symptoms with your doctor.
Image courtesy of Emily M. Eng