An In-depth Interview with Kris Newby, Author of “Bitten”
“We need to let the NIH know that we’re watching them, and we want results.”
– Kris Newby
 Kris Newby, author of ‘Bitten,’ is investigating government spending on Lyme disease research, which is strongly influenced by the flawed original disease definition of Lyme disease. She summarizes the impact of the 2018 Tick-Borne Disease Working Group’s report, explains where research funding has and is currently being directed, and calls for money to be spent on better diagnostics and treatments for Lyme disease sufferers instead. Kris explores potential actions that Lyme patients can take to help direct the course of funding, such as communicating with Congress, supporting advocacy groups, and donating to research organizations.
Kris Newby, author of ‘Bitten,’ is investigating government spending on Lyme disease research, which is strongly influenced by the flawed original disease definition of Lyme disease. She summarizes the impact of the 2018 Tick-Borne Disease Working Group’s report, explains where research funding has and is currently being directed, and calls for money to be spent on better diagnostics and treatments for Lyme disease sufferers instead. Kris explores potential actions that Lyme patients can take to help direct the course of funding, such as communicating with Congress, supporting advocacy groups, and donating to research organizations.
The views and opinions expressed in this article are those of the interviewee and do not necessarily reflect the views or positions of Bay Area Lyme Foundation.
Kris Newby is watching our government, and watching quite closely. She has a lot to say about how government money is spent on a disease that, according to CDC estimates, infects almost 500,000 people annually in the US, causing untold pain, suffering, loss of livelihood, and, in extreme cases, severe mental illness, including suicidal and homicidal events.
Of course, we are talking about Lyme disease—the pariah of infection-associated chronic conditions.
“Lyme disease—the causative organism—was discovered 43 years ago, and we still don’t have a good test or a treatment,” Kris notes. She is frustrated by this fact. Kris has dedicated months of the last three years to understanding what is happening at the highest levels of US public health institutions, the government organizations charged with caring about our health, and investing in research to alleviate disease. “Let’s compare Lyme to what happened with COVID-19,” she begins. “A little over a year after this new organism showed up, we had reliable diagnostic tests and treatments. So if there’s a will, there’s a way. And, for some reason, the world does not have the will to fix the Lyme disease problem,” Kris sighs, not hiding her disappointment.
“For some reason, the world does not have the will to fix the Lyme disease problem.”
– Kris Newby
Following the Money Reveals Minimal Funding for Lyme Treatments
However, Kris is channeling her energy around this frustration to do what she’s good at: Investigating. She’s been analyzing the publicly available information on National Institutes of Health (NIH) grants, and learning how money is being spent on less urgent projects—despite guidelines for grant funding from a federally mandated committee. Diving into the types of grants and funding categories that the NIH has put into Lyme disease in the last decade reveals how Lyme patients continue to be let down by the NIH.
“Right now, I’m finishing up the analysis of 11 years of NIH grants. That’s over 800 grants. And I’m reading the abstracts of the new ones,” Kris explains. “Two years ago, I read the abstracts of the other 600. We have an estimated two million people living with Lyme disease in the US today because the treatments aren’t working. Yet, the NIH has allocated only 2.5% of the Lyme disease research budget (2013–2023) to treatment studies—treatments Lyme patients desperately need.”
“The NIH has allocated only about 2.5% of the Lyme disease research budget to treatment studies—treatments Lyme patients desperately need.”
– Kris Newby

Why the Original Definition of Lyme Disease Still Matters
Congress allocated an average of $32M per year for Lyme disease research over the last 11 years, which is small compared to budgets for other diseases like malaria and HIV/AIDS.
Even so, this relatively small amount of money that is spent on Lyme would be effective if it was granted to researchers targeting the problems Lyme patients care about—namely diagnostics and therapeutics. But because of the arcane history around the disease definition for Lyme, most of the funds allocated to approved projects keep going to what Kris describes as: “basic research—looking at cellular processes or exploring tick biology—none of which is helping patients get better.”
Kris adds: “We need to be looking at root-cause cures, not ways to reduce joint swelling.”
The Graying of Lyme Researchers
According to Kris, there are structural flaws in the NIH’s grant awarding process that tend to favor the old guard over young researchers with new ideas. She illuminates the systemic challenge by describing the key people in the mix: “The ‘gray hairs’ responsible for the early, flawed definition of Lyme disease are still in positions of significant power and influence, sitting on grant review committees and journal editorial boards. They’re still running labs at prestigious universities, and years ago published 200-300 articles that say Lyme disease is rashes and swollen joints, easy to treat, and easy to cure.”
The NIH gave 13% of the Lyme budget to 8 of their own researchers in (2019–2023), with 3 of them above retirement age (68, 75, and 77 years).
– Kris Newby
According to Kris’s research, 12 NIH bench scientists controlled 15% of the total Lyme budget in the last 11 years (2013-2023), and half of them are now 68 to 79 years old. “When I look at this, I get frustrated,” she says. “Forty-three years after this bacterium was discovered, we still have ineffectual testing and treatments. I don’t think taxpayers are getting their money’s worth.”
NIH Grant Committees—Out of Touch with Patient Needs?
“Forty-three years after this bacterium was discovered, we still have ineffectual testing and treatments. Taxpayers are definitely not getting their money’s worth.”
– Kris Newby

An example that Kris uses to illustrate the disconnect is what happened with the Tick-borne Disease Working Group (TBDWG), formed as a result of the 2016 21st Century Cures Act. She explains: “The TBDWG was supposed to be a remedy, a way to have patient advocates communicate to the people that allocated the dollars and did the research. It was a combination of researchers, NIH and CDC people, and patients. But the Tick-borne Disease Working Group had absolutely no overlap in personnel working on the NIH strategic plan.”
This proved to be a major disconnect between the TBDWG and those in the NIH charged with action. In 2018, the Tick-borne Disease Working Group listed 23 research priorities for the NIH (see table), including investing in more accurate diagnostics and better treatments for Lyme disease patients in their report. Despite recommendations from this federally-mandated advisory committee, the NIH only addressed 6 of these identified research priorities in their 5-year strategic plan for tick-borne disease research.
Kris’s analysis of the types of projects NIH chose to fund reveals that grants were awarded to their own NIH bench scientists for basic research projects that have yielded no direct patient benefit. “And, after the 2018 TBDWG report was published, NIH funding in the categories that Lyme patients care about most (better tests and treatments) went down or stayed flat,” said Kris.
“After the 2018 TBDWG report was published, NIH funding in the categories that Lyme patients care about most went down or stayed flat.”
– Kris Newby
For 40+ Years, NIH Seems to Ignore Lyme Patients
NIH’s reluctance to address chronic/persistent Lyme patients’ health needs and channel much-needed funding into treatments seems to run counter to the organization’s mission, which is: “…to enhance health, lengthen life, and reduce illness and disability.”
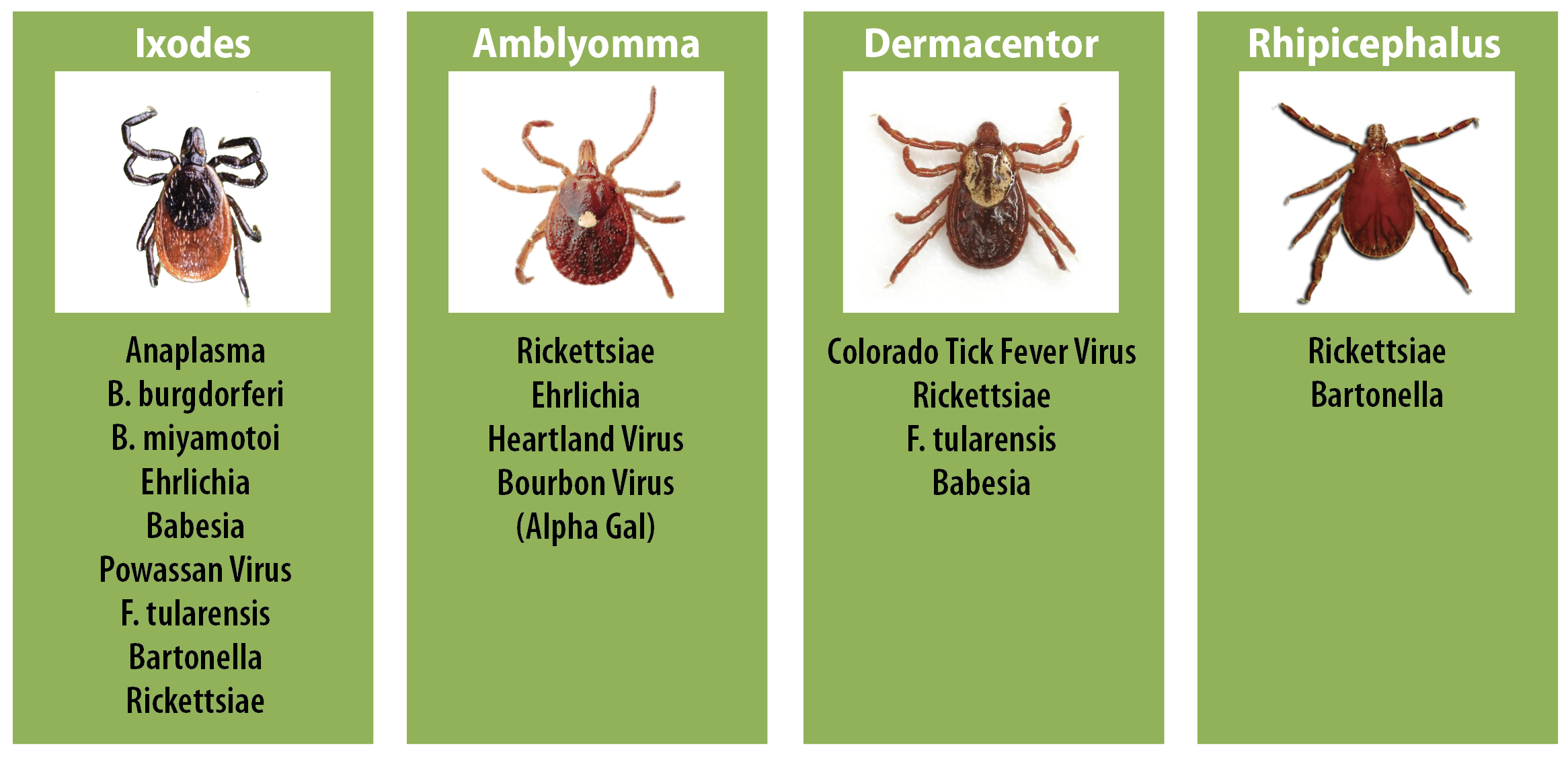
Considering that the causative agent of Lyme disease was discovered in 1981, it is curious to see the lack of funding for this particular group of illnesses. “There are at least 13 illnesses caused by 18 known tick-borne infectious pathogens,” Kris notes. “And we know that at least 10 to 20% of patients treated early fail treatment. In the later stages of the disease, treatment failure rates are higher. The Lyme community desperately needs diagnostic tests and treatment protocols that work and are rapid. We do not have that right now after 40+ years. And if they could do it with COVID, they can do it with Lyme disease.
Calls to Action: How Lyme Patients Can Be Heard
Rather than feeling defeated by her exhaustive and illuminating analysis, Kris is galvanized into sharing her findings with the Lyme community because understanding the numbers enables all Lyme patients to see, name, and communicate the problem.
Kris Newby’s blueprint for action is as follows:
- Review the graphs and statistics in this blog. They shine a spotlight on the challenge: There is a lack of mission-critical research because NIH funds are being diverted to basic Lyme science projects rather than improving diagnostics and therapeutics.
- Engage with your Congresspeople and Congressional advocacy groups like the Center for Lyme Action so we can stay involved in the important collaborative process of getting funding for Lyme disease.
- Support organizations like Bay Area Lyme Foundation. Among its many other programs and activities, Bay Area Lyme gives seed research money to young investigators with bright ideas. Researchers need proof-of-concept data to get NIH grants, and Bay Area Lyme provides money for early-stage projects that the NIH is unlikely to fund.
“Bay Area Lyme Foundations has invested more money over the last ten years in research for therapeutics than the NIH.”
– Kris Newby
For Lyme patients wanting to stay informed about NIH investments into the infections that impact them directly, Kris Newby is someone well worth following. By shining a light on this publicly available information and making it understandable and accessible to the Lyme community, we can learn how to move together to make a difference.
Bay Area Lyme would like to acknowledge the NIH for its recent grants to these researchers, whom we have also funded for their innovative projects focused on accurate diagnostics and novel therapeutics:
Linden Hu, MD, Tufts University
Michal Caspi Tal, PhD, MIT
Brian Crane, PhD, Cornell University
Monica E. Embers, PhD, Tulane University
Brandon Jutras, PhD, Northwestern University
Jacob Lemieux, MD, PhD, Harvard University
Artem Rogovkyy, DVM, PhD, Michigan State University
Janakiram Seshu, PhD, University of Texas, San Antonio
Rafal Tokarz, PhD, Columbia University
 Kris Newby is an award-winning science writer and the senior producer of the Lyme disease documentary ‘Under Our Skin,’ which premiered at the Tribeca Film Festival and was a 2010 Oscar semifinalist. Her book ‘Bitten’ won three international book awards for journalism and narrative nonfiction. She has two degrees in engineering: a bachelor’s degree from the University of Utah and a master’s degree from Stanford University. Previously, Newby worked for Stanford University, Apple, and other Silicon Valley companies. www.krisnewby.com
Kris Newby is an award-winning science writer and the senior producer of the Lyme disease documentary ‘Under Our Skin,’ which premiered at the Tribeca Film Festival and was a 2010 Oscar semifinalist. Her book ‘Bitten’ won three international book awards for journalism and narrative nonfiction. She has two degrees in engineering: a bachelor’s degree from the University of Utah and a master’s degree from Stanford University. Previously, Newby worked for Stanford University, Apple, and other Silicon Valley companies. www.krisnewby.com
This blog is part of our BAL Spotlights series. More in-depth analysis regarding NIH spending on Lyme disease to come! Information on NIH grants awarded for research into Lyme and tick-borne diseases was taken from documents that are available in the public domain. Stay up-to-date on developments by subscribing to our newsletter. Contact us if you require a copy of this article in a bigger typeface and double-spaced layout. Bay Area Lyme Foundation provides reliable, fact-based information about Lyme and tick-borne diseases so that prevention and the importance of early treatment are common knowledge. For more information about Bay Area Lyme, including our research and prevention programs, go to www.bayarealyme.org.
References:
 We wish to thank Kris Newby for her time and effort in bringing this valuable information to light. The views and opinions expressed in this article are those of the interviewee and do not necessarily reflect the views or positions of Bay Area Lyme Foundation.
We wish to thank Kris Newby for her time and effort in bringing this valuable information to light. The views and opinions expressed in this article are those of the interviewee and do not necessarily reflect the views or positions of Bay Area Lyme Foundation.